By: Cristina Spears, Marketing Manager
October 6th, 2024, Marks the two-year anniversary of the information blocking rule (IBR).
Patients have never had this degree of access and control over their medical records!
In the history of U.S. healthcare, a patient’s access to their medical record data has never had the level of liquidity that exists today. A bold statement, but it is a fact! An individual’s right of access to their EHR data (technically defined as electronic health information or EHI) is not optional, it’s mandated under the Cures Act and Information Blocking Rule (IBR). When access is restricted because of interference by a provider or an EHR vendor, this is now enforceable with penalties.
In this article, we will examine what changes have taken place since the two-year anniversary of the Information Blocking Rule (IBR) and the impacts to date. Clearly, we are still closer to the starting line than the end game of healthcare data interoperability and power shift to the patient. However, we are optimistic and excited about what lies ahead!
Are we there yet?
Let’s break down a few key details:
Purpose: The Information Blocking Rule aims to promote the interoperability of health information systems and ensure that patients have access to their health information without unnecessary barriers. It is intended to prevent practices that block or impede the sharing of electronic health information, thereby improving patient care and health outcomes.
Scope: The rule applies to a broad range of healthcare entities including healthcare providers, health IT developers, health information networks, and health information exchanges.
Key Provisions:
- Definition of Information Blocking: The rule defines practices that are considered information blocking and establishes exceptions where practices are not deemed to be blocking.
- Exceptions: The rule outlines several exceptions to the information blocking prohibition, such as practices that are necessary for patient safety, privacy concerns, or legal obligations.
- Enforcement: The Office of the National Coordinator for Health Information Technology (ONC) and the Office of Inspector General (OIG) are responsible for enforcing the rule. Penalties can include fines and other corrective actions.
Reflecting on where we were as an industry before the IBR compared to where we are today, there has been a tectonic shift in power to the patient in terms of what is in the regulations. With that said, most patients do not fully realize they have this power yet. On the ground there are signs of this power shift as EHR vendors have provided the capability which enables patient access and sharing of EHR data. Epic is the best example of an EHR vendor that has made it easy for patients. Why? Compliance with the IBR, and recognition that market share and risk tolerance go hand in hand. Epic has more IBR exposure than any other vendor by far. It can be very risky business for EHR vendors when they do not comply with the rules, and Epic clearly knows this.
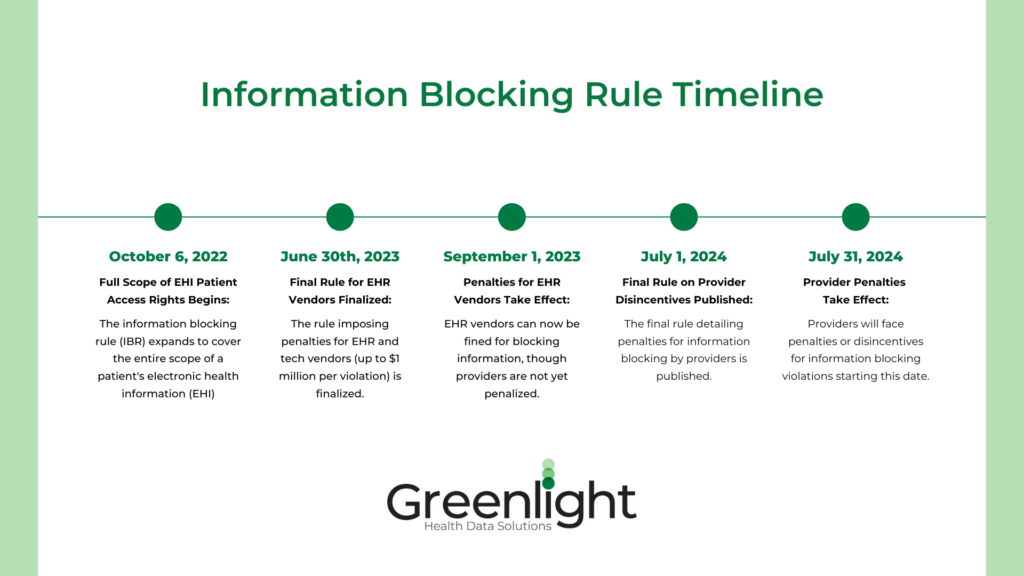
We celebrate the two-year anniversary, but there are some important dates that have not had as much attention as they certainly should.
While the IBR created the requirement on Providers and EHR vendors and the right of access for patients, it was without teeth or penalties for non-compliance until much later. The rule was a promise made that would be kept but could not fully be counted on until the enforcement regime was enacted.
On June 30th, 2023, the final rule that included penalties for information blocking by EHRs and other technology vendors (up to $1 million per occurrence) was finalized with an effective date of September 1, 2023. In other words, an EHR vendor could block on August 31st, 2023, and be in violation, but they could not be penalized in any way. So, the promise was kept, but Providers could potentially block access since they had no negative impacts or penalties from doing so.
On July 1, 2024, the final rule on disincentives for information blocking by Providers was published with an effective date of July 31, 2024.
Disincentives can include (drastically summarized):
- Posting and release of information about specific violations by Providers after full review and final determination on any instance(s). Wall of shame type approach.
- Potential for removal from Medicare specific incentive programs participation and, as a result, reductions in payment incentives and rates.
Once the given penalties were fully in place, the benefits could accelerate.
While the Patient has the power, it’s the authority of the federal government (HHS-OIG) to enforce the rules of interoperability. More than just alphabet soup, the HHS reorganization and renaming of the ONC to the Assistant Secretary for Technology Policy and Office of the National Coordinator for Health Information Technology (AST/ONC) establishes new roles for a Chief Technology Officer, Chief Data Officer, and Chief AI Officer. The expanded responsibilities of AST/ONC and creation of these roles are vital in supporting the mission and vision of The Federal Health IT Strategic Plan over the next six years. The top purpose listed for this strategic plan – “individual access to EHI” – reinforces the power of the Patient.
What Happens Next
Patient access to EHR data is more liquid than any point in the history of healthcare, so what happens next? EHR data liquidity continues to accelerate for patients, and they begin to realize this through convenient functionalities that are layered in by EHR vendors to support advancement in interoperability
Today, patients legally have access to their EHR data any time they need it, but only some know it and how to access it. Most patients know very little about healthcare interoperability and assume this automatically already happens. In addition, many external industry participants (non-treatment use cases) have yet to realize the potential of leveraging this power to drive cost savings, efficiency, and customer experience. At Greenlight, we know this and, as an agent to the patient, we support going the extra mile to make it easy for patients to share their data. For our partners, we bring data liquidity to processes that are largely dependent on paper, email and fax machines.
Call to Action
Choose to celebrate the two-year anniversary of the Information Blocking Rule because it drives the potential for innovation across the industry. It is a big win for control over health information, a right that we as patients should have always had. How crazy would it be if you didn’t have access to your own financial information to make investment decisions? The same logic applies to our right to have immediate access to our health information to get, for example, a second opinion on a proposed high-risk surgery.
Greenlight Perspective
Greenlight’s EHI data sharing APIs support connections to over 90% of the U.S. provider market. We’ve been advocates for an individual’s right to access their health information throughout our 25 years in the healthcare IT industry and now federal legislation makes that access a reality.
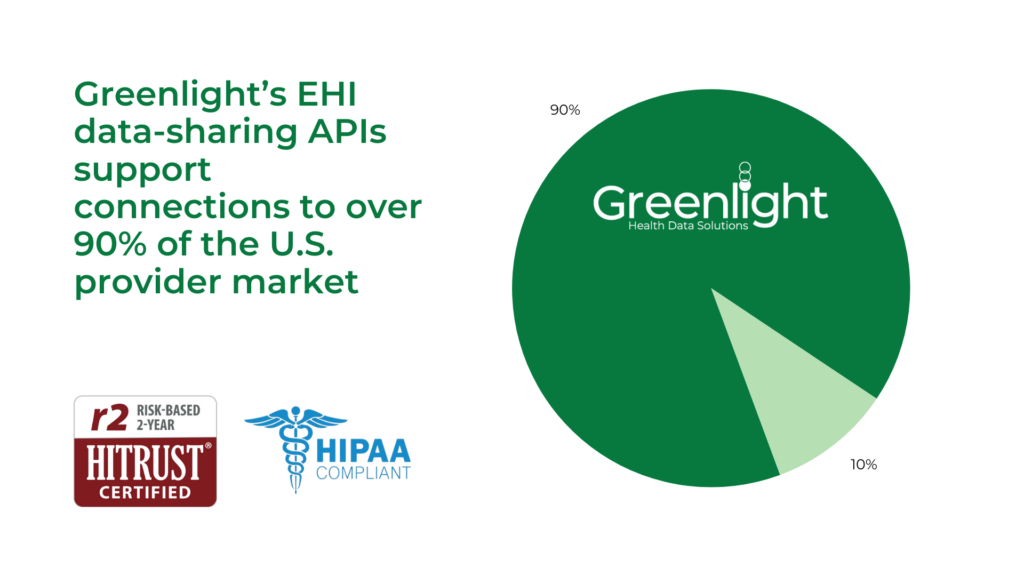
Capturing the patients’ informed consent to share their EHI data and ensuring that the data is not used for other purposes outside consent is foundational to what we do.
The Greenlight platform connects patients, healthcare providers, insurance companies, and life science organizations. Say goodbye to antiquated, paper-based processes and hello to a new era of patient-first healthcare.
Join us to expand a patient health record revolution across industries.
Patients: Control what records are sent securely and quickly.
Providers: Obtain patient-authorized medical records in minutes.
Researchers: Accelerate innovation and improve efficiency across medical research and clinical trials.
Insurers: Revolutionize how your firm uses patient health records.

We are empowering patients to control their digital health data records so that leading companies can deliver innovation in the services they provide.
Contact us about how you can benefit from Greenlight Health Data Solutions logical and intuitive workflow: https://greenlighthealth.com/contact/
Sources:



